| |
Page 1:
What’s New
Basic Overview
Page
2:
Photosensitizers
Page
3:
Photosensitizers continued
Page
4:
Light sources
Applications of PDT
References
Contact information
|
|
 |
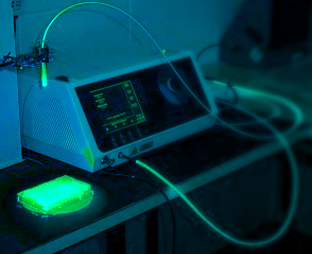
One of the limitations of PDT is its dependence on the accessibility
of the light delivering system. Recently Light Emitting Diodes (LEDs)
and florescent lights have been used because of their convenience of
use but laser light still remains the primary light source for PDT (Fig.5).
Though cumbersome laser light devices have strong advantages over other
sources by emitting light that is “monochromatic (exactly one
colour), coherent (light waves are parallel permitting precise focusing),
and intense (allowing for shorter treatment time)”. (2)
|
 |
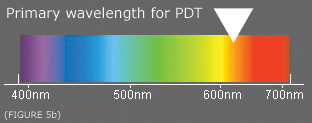 |
Figure
5. One of the preferred sources of light still remains
to be laser light because of its monochromatic nature, coherency
and intensity. Wavelengths most efficient at tissue penetration
is around 600-700nm (Fig. 5b) and is within the
red end of the visible spectrum.
|
|
 |
A typical PDT treatment involves application a light sensitive drug
(containing photosensitizer) applied as a cream for treatment of skin
cancer or injection for other cancers. A delay is given to allow the
photosensitizer to localize in targeted tissue. Following the delay
light is applied the targeted region. The light source used is a non
burning light source which does not affect the surrounding normal cells.
For skin Cancers the light can be shone directly onto the skin but for
internal Cancers a flexible tube light source is inserted into the patient’s
body.
Current
uses of Photodynamic therapy include treatment of early malignancies,
Cancers of the esophagus, lung, bladder and basal/squamous cells. Other
non-Cancer related uses include treatment of acne, age related macular
degeneration and plaque psoriasis.
Photodynamic
Therapy is most efficient when treating early malignancies. For cases
involving advanced cancer it is used only to help reduce symptoms. To
actually cure cancer in its advanced stages photodynamic therapy must
be combined with other methods of therapy such as chemotherapy.
|
 |
Figure 6. An example of the Light Emitting Diodes (LEDs)
probe used in brain cancer therapy. Light produced is approximately
three times greater then that of the sun. (7)
|
|
Side
effects of PDT include pain, swelling and sensitivity to light. Patients
are advised not to expose themselves to sunlight or bright indoor lighting
for four to eight weeks after treatment. Exposure to bright light causes
severe sun burning.
Pain associated with PDT is mild and is the result of the break down
of targeted tissue. Unlike other therapies, PDT does not cause cumulative
damage (e.g. radiotherapy or chemotherapy) and therefore patients can
be repeatedly treated.
|
 |
(1)
Hasan,T and Moor, A.C.E and Ortel, B (2000). Photodynamic Therapy of
Cancer. Cancer Medicine fifth ed..36, 489-510.
(2) Gagel, P. (1997). Photodynamic Therapy with Porphyrins.
Derm Web at UBC. http://www.dermatology.org/laser/pdt.html.
(3) Pavia, Lampman, Kriz (2001). Principles of Absorption
Spectroscopy. In Introduction to Spectroscopy, Third edition, chapter
7.2, pp. 355-356. Bellingham: Harcourt College Publishers
(4) http://www.bmb.leeds.ac.uk/pdt/science.htm
(5) Su, F. (2000). Photodynamic therapy: a maturing
medical technology. OE Reports. http://www.spie.org/web/oer/february/feb00/phototherapy.html
(6) http://www.bccancer.bc.ca/HPI/drugdatabase/drugindexalpro/porfimer.htm
(7) Nelson,D. and Cox, M. (2000). Lehinger Principles
of Biochemistry. Third edition, chapter 7, pp. 204-205. New York: Worth
publishers
|
| |
BACK | HOME | |
Chem
321 Report; By Ryan Martinez,230029611; Please contact me with any comments:
knee_pole@hotmail.com
|





