|
|
| |
| Causative Agent |
-
A
tick-borne, potentially
zoonotic, disease primarily of
rodents and
lagomorphs. Caused by the
bacteria, Francisella tularensis.
-
Two different sub-species of
F. tularensis:
-
one holarctic (F. t.
palaearctica);
-
one restricted to North
America (F. t. tularensis).
|
| Images |
|
Click on
images to enlarge. |
 |
 |
|
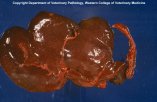
Small white dots of necrosis
on the liver of this beaver are typical of tularemia. |
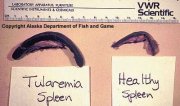
Enlargement of the spleen is
typically observed in animals with tularemia. |
|
| Distribution |
|
Geographic: |
-
In North America:
-
F. t. tularensis
occurs in terrestrial
habitats;
-
F. t. palaearctica
occurs most often in aquatic habitats
(wetlands and boreal areas).
-
F. t. tularensis
does not seem to occur in
Canada and may be limited to the lower 48 contiguous United
States.
-
F. t. palaearctica
infection primarily occurs
in Canada.
|
|
Seasonality: |
-
Ticks
are
only present on hares from May to September (based on Alaska
data); as a result, the disease essentially disappears from
October through April.
-
Human cases may also occur throughout the fall and winter
following exposure to
lagomorphs during hunting season.
|
|
| Hosts, Transmission and Life
Cycle |
| Hosts: |
-
F. t. tularensis: rodents and
lagomorphs.
-
F. t. palaearctica:
aquatic rodents.
-
In North America, tularemia occurs most commonly in cottontail rabbits (Sylvilagus
spp.), muskrats (Ondatra
zibethicus), ground squirrels (Sciuridae), and beavers (Castor
canadensis).
-
It is thought that tularemia is often fatal in the above species, but not
so for the snowshoe hare (Lepus
americanus).
|
|
Transmission: |
-
F. t. tularensis:
transmission occurs among hosts primarily through
ticks, but
also by
mites,
mosquitoes, fleas,
lice and
biting flies (Tabanidae).
-
F. t. palaearctica:
transmission occurs directly through water, which may remain
infectious for weeks to months following contamination.
-
For
both sub-species, transmission may also occur through contact
with feces, urine or body parts of infected animals.
|
|
Life Cycle: |
-
Although often fatal, the
bacterium can infect both
lagomorphs and rodent hosts without
apparent ill-effects. These hosts can then remain infected
for extended periods, serving as
reservoirs of infection for other animals and
biting arthropods.
-
Ticks
act
not only as
vectors of transmission, but also
as
reservoirs of the
bacterium, which can live in certain
tick species for months.
-
F. t. palaearctica
may
also be transferred among voles (Microtus spp.)
through cannibalism of infected individuals.
-
The
associations between mammal and
arthropods differ from location to
location.
|
|
| Signs and Symptoms |
|
Animals: |
-
In the most sensitive
species,
clinical signs are not often observed due to the short duration of
infection before death occurs. These animals are usually in good
body condition at death.
-
In less sensitive species, during the latter stages of
the disease, animals may become lethargic or depressed and have
elevated body temperature.
-
Tularemia is most often recognized during examination
at a
diagnostic laboratory.
-
Tiny, pale spots on the liver, spleen or lung are
typical
lesions of
tularemia.
-
Spleen or liver may become enlarged.
-
As
in humans, an
ulcer may
form where the
bacteria have entered the body.
-
Thin, whitish strands of material may be present in the
abdominal cavity.
-
The
lesions
described above are not unique to tularemia: see also
plague.
|
|
Humans: |
-
Initially, symptoms
are: generalized fever-like illness (e.g., fever with chills,
headache, vomiting) beginning 1-10 days after infection.
-
Confirmation of the
disease is usually accomplished using blood tests.
-
The course of the
disease depends on the route of infection:
-
arthropod
bite: an
ulcer
forms at the bite wound followed by enlargement of the
lymph nodes draining the area of the bite wound;
-
inhalation: inhalation of infected material results in
pneumonia;
-
ingestion: infected water or meat that is ingested
leads to
inflammation of the posterior portion of the oral cavity and
intestines.
-
Disease resulting from F. t. tularensis is more
serious than that caused by F. t. palaearctica.
-
Death occurs in 40-60% of untreated cases
where
pneumonia or
inflammation of the inner surface of the intestines
occurs, and 7% of all
forms of untreated infection with F. t. tularensis. In
contrast, fatalities occur in 1% of untreated infections with F.
t. palaearctica.
-
Human to human transmission is rare.
-
F. t. palaearctica
is
common in trappers.
|
| Meat Edible? |
-
Normal cooking
temperatures destroy
bacteria in
the meat; it is, therefore, safe to eat when thoroughly cooked.
-
Human exposure typically results from preparing carcasses.
|
| Human Health Concerns and
Risk Reduction |
-
Human infection in
North America prior to 1950 has been closely associated with
exposure to cottontail rabbits infected with the F. t. tularensis
strain.
-
After 1950, the major
risk factor to humans has switched to muskrats infected with the
F. t. palaearctica strain.
-
Taking certain
precautions can reduce the chance of exposure to the tularemia
bacteria,
such as: basic hygiene, use of insect repellents and
protective clothing to avoid
arthropod bites, inspection and removal of
ticks,
use of gloves when handling and dissecting wild animals,
particularly rodents and
lagomorphs.
-
Vaccination against tularemia may be warranted in
high-risk areas.
-
Dogs and cats can die from tularemia. Since infected
animals are easier to catch, pets may become infected after eating
the internal organs of the diseased animal. Keeping pets from
roaming free should help to reduce the spread of tularemia.
-
Tularemia is readily treated with antibiotics if
treatment is started early in the course of the disease. Thus,
symptoms of general malaise and fever should not be ignored and
medical attention sought. Medical personnel should be advised that
you may have been exposed to wildlife and so may be at risk with
respect to various wildlife diseases including tularemia.
|
| Samples for Diagnosis |
-
Submission of entire
carcass or just the spleen or liver.
|
| Similar Diseases |
-
Lesions in animals
infected with
plague,
yersiniosis and other
bacterial infections may be similar to that of tularemia.
|
| Further Reading |
|
|
|
|